Historian Emily Mayhew meets soldiers who have survived the seemingly unsurvivable, describing the moment of their wounding, and what happens next in her book A Heavy Reckoning, War, Medicine and Survival in Afghanistan and Beyond. Headley Court in Surrey has been the centre of military rehabilitation services since the Second World War. Here, she explores the part prosthetics play in that process.
Sockets and stumps
Words by Dr Emily Mayhewaverage reading time 6 minutes
- Book extract

A Headley patient’s first stay usually lasted 24 days. When the physios and everyone in the team agreed, people from the prosthetics department arrived, and that was always a very good day.
Prosthetics are the artificial substitutes for parts of the human body that are missing. Prosthetics can be permanently implanted (teeth, facial bones, hips, knee joints) or removable (hand, arm, leg). Prosthetic legs represent the greatest challenge to both builder and wearer. Legs need to be load-bearing, to carry their wearer forward, to get them up and out of the chair for as long as possible.
Other prosthetics do other things for their wearer, but none has quite the same impact, or quite the same level of technical difficulty, as getting them up and out of their wheelchair.
Prosthetics in one form or another have been around as long as human beings have had the wit to build them. For most of lost-limb history, they’ve been made of wood, carved to shape and lumped around, strapped around whatever is left of the body part they were meant to replace.

An artificial left leg with thigh socket from the 1920s.
The modern prosthetic leg, jointed and with metal and wood parts as we would recognise it today, evolved for the two largest amputee cohorts produced in war: 38,000 from the American Civil War and (in Britain) 41,000 from the First World War.
War didn’t just produce amputees and legs for its casualties; it also produced prosthetic limb industries – workshops, research, design studios, manufacturing and fitting. And durable limbs as well as organisations. Many of the companies that were successful in the nineteenth and twentieth centuries are still market leaders today in the twenty-first (more about one in particular later).
Today most people know about the extraordinary gains in prosthetic technology from events such as the Paralympics, where materials and design technologies are brought together to produce performance limbs for superhumans.
MORE: You, a thousand years ago
Prosthetic limbs, and in particular prosthetic legs, have come to represent everything we know about dealing with amputation.
This isn’t quite right, because the limb that we can see is only the end, not the means whereby amputees are able to function. Also, because despite all the research and development and superhuman efforts, prosthetic limbs don’t work as well as we would like.
A design historian summed this up elegantly (as design historians are wont to do): ‘of all machines [the artificial limb] has the closest proximity with the human body but the least chance of matching its performance.’
The primary reason for the generally sub-optimal performance of artificial limbs is not the artificial limb itself but the stump on to which it fits. It fits on to the stump by means of a socket, and it is this system that is at the heart of limb replacement. (Which is why this article is called ‘Sockets and stumps’ rather than ‘Prosthetic legs’.)
Meanwhile, back to the team meeting at Headley where the amputee first met the prosthetics department (a private company, Blatchfords, by the way, founded in 1890 and greatly expanded during the First World War, responsible for a model of leg prosthetic named ‘The Clapper’, because that was the sound it made when fully extended; at least the models are silent now).
In the twenty-first century the prosthetist took the bandages off their patient’s stumps and looked really closely at them, handling the stumps in a different way from everyone before, as something to work with, with potential.
If there was no infection, and they were healing normally, and the work in the gym was going to plan, then they came back with a load of kit, including a bucket full of plaster cast. Then they covered the stumps in cling film and took a plaster cast mould.
Legs

This artificial left leg is made from willow and leather. Earlier versions were known as ‘Clapper’ legs after the sound the leg made when fully extended.

The leather corset at the top of this left leg secures the prosthesis to the thigh. It's perforated so the wearer doesn't get too hot. Inside the calf is a v-shaped metal bar attached to a spring. This prevents the wearer falling forward, but allows them to walk with comfort. The ankle and knee joints are lockable, and the toes are made of flexible leather.

Prosthetic legs like this one from 1914-20 were known as pylons. They were issued to servicemen who had recently lost a leg to get them used to the idea and feel of an artificial leg. They would be worn for a short period before a proper artificial limb was fitted. Made from fibre with leather padding, the leg was issued by a Red Cross provisional limb depot in Stretford, Manchester, England.
In the prosthetists’ workshop, where they do more of these for highly demanding, impatient humans than anywhere else in the country, they think that plaster cast moulds are still more efficient than a digital scan and 3D printed models. So far, even the best computer scanner isn’t a match for a really experienced prosthetist with an artist’s eye and a set of fine files to reshape carefully until the fit is as good as it can be.
The kit associated with making plaster casts can make the prosthetic workshop look like a sculptor’s studio. There are five prosthetists at Headley, and they all have white plaster residue in their fingernail beds and knuckles, and they all make very slightly different-looking casts, so anyone who knows how they work can tell who built which model, like telling a Michelangelo from a Bernini.
In the workshop they make a hard-plug solid replica of the stump. And from the solid replica they make a bucket-shaped object that slots over the stump: a socket. Everything comes down to this piece of machinery, a socket, carefully honed to fit a human, and to the moment when it is first handed over (and it’s heavier than it looks – as heavy as the original body part it is to replace because that’s what the central nervous system is used to).
They are not handing over a leg. They are handing over the means to a leg. The dictionary says a socket is a natural or artificial hollow for something to fit into or stand firm, or that can be used to make a connection.
Hands and arms

A prosthetic hand and forearm dating from 1890. It’s made from steel, with brass wrist mountings and a leather upper arm socket

This prosthetic left arm from 1927 has a canvas coated hand to give the appearance of a gloved hand. The fingers of the hand are set in position, but the joints of the arm are adjustable and the hand is removable. Aluminium was preferred to wood as it was much lighter and was more comfortable for the wearer. As such it is one of a new generation of metal limbs that appeared in the 1920s and which gradually replaced the predominantly wooden ones.
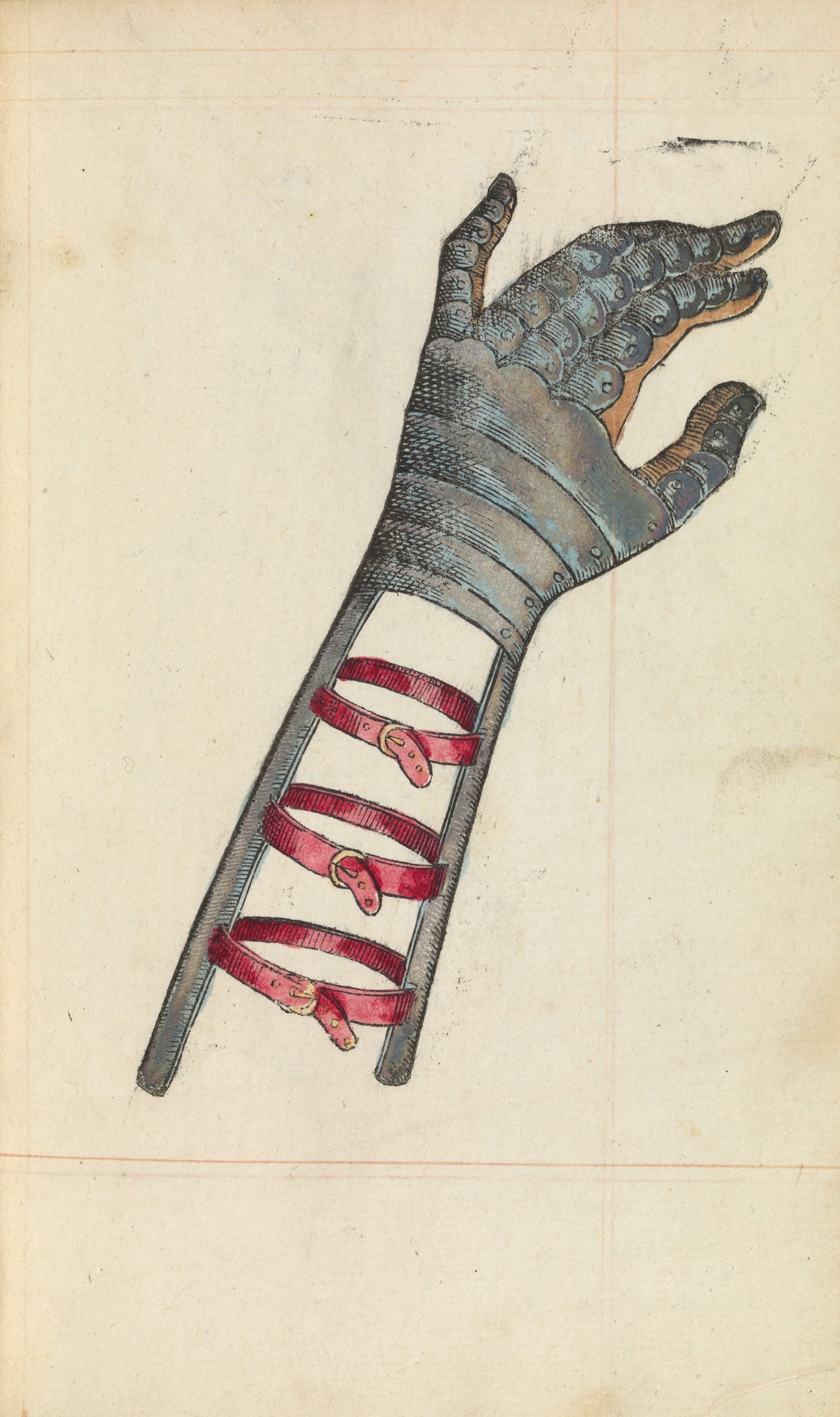
A hand-painted wood engraving of a prosthetic hand by Ambroise Pare, 1564.
Sockets aren’t just about something to clip a limb into. They restore evenness of length to limbs, because blast injury rarely gives them anything neat to work with.
Stumps are of different volumes, different widths and different lengths. Sockets have inner linings that even things up and make things steady. An amputated thigh bone (femur) floats about in the soft tissue of the thigh itself, without muscles and ligaments to hold it effectively where it should be.
So the socket has to fit closely over the stump and give shape, structure in such a way that the whole thing is made stable, with no more floating about, doing damage. The socket needs to be not too tight and not too loose: just right to hold the stump in a new place, firmly, all the time.
Part of this stability is about the weight of the rest of the body and how that comes down on to the stump. Bone that has been cut through can’t take weight, so the socket is designed to take the weight of the body and distribute it back to areas with soft and hard tissue intact. Generally, this means the weight is moved through the socket structure to areas that can carry it, such as the hips and pelvis. So each stump, even on the same patient, is different because no two stumps are ever the same.
Depending on the bone, and how the blast has blown it away, the socket may go high up the leg, almost to the hip to provide the support to the soft tissue and leftover muscles. It’s really complicated stuff, and never exactly, precisely, permanently right.
‘A Heavy Reckoning’ is out now.
About the author
Dr Emily Mayhew
Dr Emily Mayhew is a military medical historian specialising in the study of severe casualty, its infliction, treatment and long-term outcomes in 20th and 21st century warfare. She is historian in residence in the Department of Bioengineering at Imperial College, and a Research Fellow in the Division of Surgery within the Department of Surgery and Cancer. She is the author of ‘Wounded: From Battlefield to Blighty 1914-1918’, which was shortlisted for the Wellcome Book Prize 2014.
