Poet, performer and writer Jamie Hale is often admitted to hospital due to their chronic illnesses. Here Jamie exposes the underfunded home care that caused a recent spell in hospital, and the rigidity of hospital systems that often make things worse.
How hospital care fails disabled bodies
Words by Jamie Halephotography by Camilla Greenwellaverage reading time 7 minutes
- Article

In some ways, we’re all trapped when we’re in hospital. Your agency is stripped along with your clothes and you’re given matching gown, bedding, bed. Everyone looks the same.
In some ways we aren’t. The man two beds down, and furious that the surgeons might amputate his toe, can get up, walk out and go home. I can’t. I might as well be tied to the bed for all the freedom I have to move.
I am never more strongly reminded of the disobedient nature of my body than when I’m in hospital. Hospitals are designed for ill people, not for disabled people. You’d think that the needs of the two groups would overlap – I would once have thought that – but they don’t.
I am admitted to hospital quite often, and face dread each time. I know I will emerge weak, potentially malnourished, and with complications ranging from worsening contractures to severe infections.
The hospital model is based on taking ill people, treating them, and making them as well as possible before discharge. It isn’t designed for people who are trying to limit their decline with careful management and established routines. It’s built for unwell patients who need doctors to make the decisions, not disabled people who know what their bodies need.

"My body and I have reached an uncomfortable accommodation, and if I meet its needs, I can lead my life."
Rigid rules and suspicious staff
The hospital is a space for rules. How else would it function? Without the rules, things get forgotten – it’s an ecosystem bigger than any one patient – and its stability relies on those rules. In some ways those rules are simple. Measure the production of my catheter, the millilitres on my water jug, the saline in the drip. Maintain a positive fluid balance. Allow for sweating. Count the ways in which a body can break down, and the ways in which it can be recovered. The ill body is reduced to a series of processes.
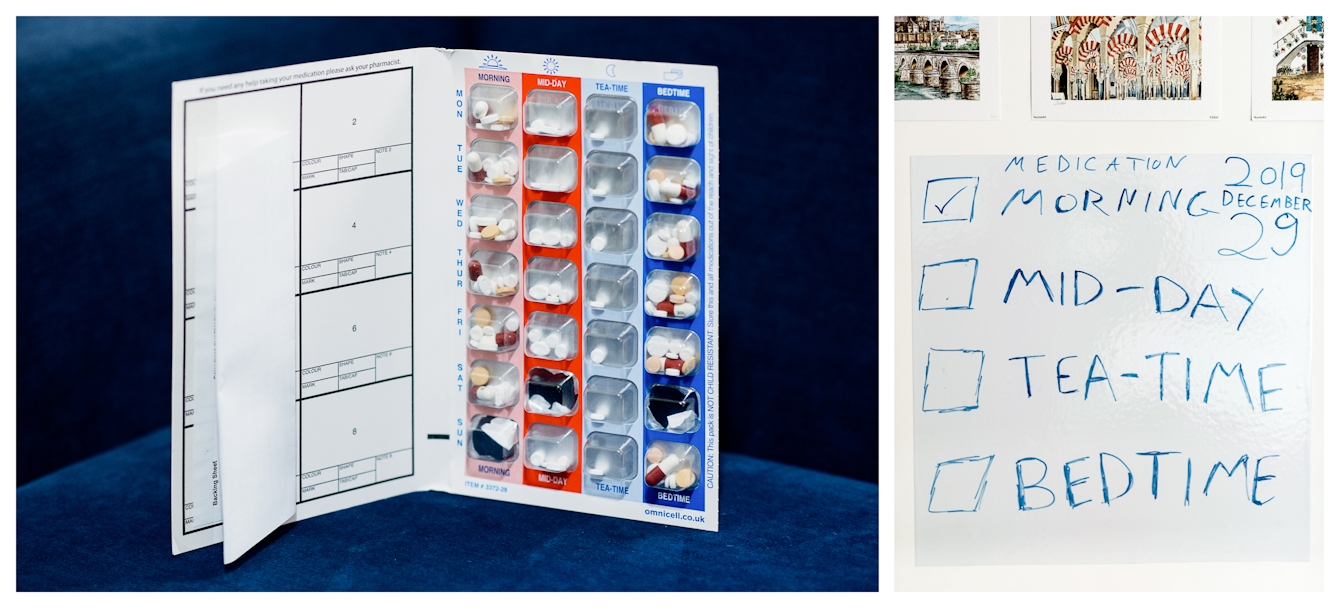
As a patient, you are no longer trusted to even narrate those processes. I have learned this many times over. I was reminded yesterday, when critical medications were signed for but not given. I repeated my request for them, and was told that they’d been given; I knew they hadn’t. My legs were twitching. It was only the fourth time I told them, when I said, “My carer doesn’t remember me having had my medication,” that they sprang into action. The voice of a carer holds weight above that of a patient.
I know my body well, better than any carer can. My body and I have reached an uncomfortable accommodation, and if I meet its needs, I can lead my life. In hospital my freedom to meet those needs is sharply curtailed. If I need medicine, I must buzz, wait half an hour, ask for a nurse, wait again, get the medicine, ask them to help me take it, take it, and then somehow I’ve lost 90 minutes to pain and spasms.
“In a hospital, I can’t possibly have doses early, because medication happens at certain times.”
And I worry they see me as non-compliant. Asking for things their system can’t give. When your body misbehaves, you feel responsible for controlling it. I rein my legs in as best I can, but when I’m given an anti-spasmodic only every eight hours, my legs have time enough to gain some tension – muscles pulling against me. At home I usually take it three times close together, thus my legs are pliable by day. Then by night, when another medication kicks in, it hurts less when they twist and wind.
In a hospital, that control is taken away and I suffer for it. Things must be done by the book. I can’t possibly have doses early because medication happens at certain times. Nurses nod along when I explain the wire coils my muscles can become, but the chart the doctor signed says no, and the doctor is too busy to visit. They’re saving lives, not minimising discomfort. The nurse apologises, but I don’t blame them, I blame a system that can’t meet my needs.
The fear of disappearing
This time I was admitted with a serious pressure sore, and I need to be turned every two hours. This doesn’t happen. Every step that can be taken to persuade the staff to do it, it seems, has been taken. Nobody follows the procedures, and this risks another sore. As my body becomes increasingly demanding, I become increasingly quiet. I know I’m complicated enough. I ask for as little as possible.
As my body becomes increasingly demanding, I become increasingly quiet… I ask for as little as possible.
My master’s degree and my writing are my shield against disappearing. I brandish them constantly. I repeat these things in a quiet frenzy, desperate for people to treat me as somebody with a quality of life. Desperate that the staff not just see me as a shell in a bed, but as a person like themselves.

"I went home, rehydrated rectally using cut-price Dioralyte and tried to save my independence."
I summon every bit of cheeriness, chirpiness, ask about their days. I’m nice. As if the politeness of my personality will offset the costs of my body. They describe me as “inspirational” for being a disabled person doing things when many of their non-disabled patients don’t.
I try and swallow this as a compliment, and not snap that it is normal, and expected, for someone in their mid-twenties to be working. That they only think me inspirational because their expectations of what a disabled person can do are so low.
The staff are nice here, but niceness doesn’t erase the exposed wiring on my bed, the lack of pillows, the interdepartmental dispute around giving a specialist mattress to a non-geriatric patient. The nurses are lovely, open, friendly, but the wards are understaffed, and I often wait half an hour or more for the bell from my side room to be answered. Every time this terrifies me – because in an emergency I cannot get up, walk, seek help.
The staff, busy saving lives, don’t have enough time to save my skin from deteriorating again. If I am admitted to hospital with an infection, and emerge with a pressure sore, I have simply acquired another in an increasing list of complications.
On a recent admission, I waited five days for my carer to arrive and help me use the toilet, only for the staff to be too busy to hoist me. By the time I was discharged, I was millimetres from a bowel impaction. I could no longer drink or run my feeding tube. I went home, read articles on wilderness medicine, rehydrated rectally using cut-price Dioralyte and tried to save my independence. With this, medication, and care, I slowly improved. I squeaked through.
Hospitals treat emergencies, rather than daily maintenance. However, I often need emergency treatment as a result of the lack of maintenance – and so the cycle continues.

"Maybe the system will listen to me and start building the framework I need to be safe."
Dreams of the future
The future of the NHS, the media tells us, is “personalised care”. This looks at the totality of someone’s needs and develops a care plan that acknowledges it’s more practical and cost-effective to treat someone properly once than to have five different systems each doing their bit, none of them overlapping.
I dream about a system that pays for the assistance I need to turn over in bed at home so I don’t develop suppurating wounds, leaving me in hospital for weeks on end. One where I’m not a prisoner in my home because of a lack of care. The understanding that my body and I have developed gives me a happy life, but is worthless if I don’t have the support I need to live that life.
Maybe the system will listen to me, respond, and start building the framework I need to be safe. Maybe I will be at the centre of my care. Maybe I will be allowed to live the life of possibilities I desire.
About the contributors
Jamie Hale
Jamie is an artist, curator, and founder and artistic director of disability arts organisation CRIPtic Arts. They create poetry, comedy, scriptwriting and drama for page, stage and screen, and are currently directing a showcase at the Barbican Centre for autumn 2021 and a disability arts documentary. They have written for Wellcome Collection and the Guardian newspaper and have performed at venues including the Southbank Centre. Their poetry pamphlet, ‘Shield’, was published in January 2021.
Camilla Greenwell
Camilla Greenwell is a photographer specialising in dance, performance and portraiture. She regularly works with Sadler’s Wells, Barbican, Candoco, Rambert, The Place, the Guardian, the British Red Cross, Art on the Underground and Wellcome Collection.

