Maternity services. Volume II, Minutes of evidence.
- Great Britain. Parliament. House of Commons. Health Committee
- Date:
- 1992
Licence: Open Government Licence
Credit: Maternity services. Volume II, Minutes of evidence. Source: Wellcome Collection.
31/320 (page 363)
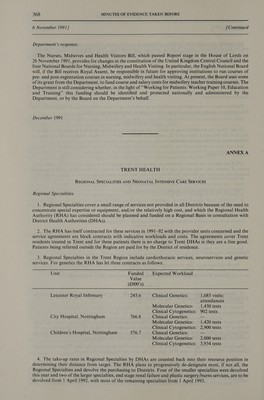
![6 November 1991] [Continued Department’s response: Clinical Standards Advisory Group The Clinical Standards Advisory Group (CSAG) has been asked by the United Kingdom Health Ministers to advise on the standards of clinical care for women in normal labour. Their investigations will include variations in clinical protocols for and practice in the management of women having their first child in a representative sample of labour wards in NHS hospitals. They will also investigate the use of corticosteroids in cases of premature labour. CSAG expects to report to the Health Ministers next Summer. Confidential Enquiry into Stillbirths and Deaths in Infancy The Confidential Enquiry into Stillbirths and Deaths in Infancy (CESDI), a unique initiative worldwide, will be a continuous programme of selecting for detailed enquiry a proportion of the around 10,000 late fetal losses, stillbirths and deaths in infancy which occur each year in England, Wales and Northern Ireland. Ministers will be advised by a National Advisory Body (NAB) about the proportions of such deaths which should be studied in any one year. The NAB will be set up shortly and will comprise representatives of professional bodies, voluntary organisations and NHS management. In 1992 the NAB will advise the NHS of the systems needed to conduct the Enquiry and the first full year’s data will be collected in 1993. A national report of findings and recommendations is expected to be published in 1994. (h) The Department’s table on current contracting arrangements for regional services for perinatal and neonatal intensive care indicates that the previously regionally funded services have largely been devolved down to district block-contracting. The data suggest that only SE Thames has top-slicing and a regional contract. However, Mr Edwards said on 6 November (Q859) “*. . . in my own particular region the services are contracted for regionally on the basis of an agreed sum which is top sliced and allocated. This is the pattern across most of the country . . .”. This appears to contradict the Department’s earlier evidence, which suggests that in Trent there is no top-slicing. Dr Walford, commenting on this later in the evidence, suggested that they do not have the power to stop small neonatal units being established. At Q879 she indicated that regions could not force DHAs to make appropriate contracts, but in Q864, Dr Walford states that the DH supports the three-tier (or two-tier) structure. How is this structure to be maintained without top- slicing anda regional contract? Department’s response: Prior to April 1991 top-slicing was used for funding neonatal intensive care and money for the service went direct to sub-regional centres from regions. Since the introduction of contracting arrangements regions have adopted a variety of approaches and, in some instances, this still involves top-slicing. The Department’s earlier supplementary note on the subject made clear that a// regions have either a two or three tier structure for neonatal intensive care, though in East Anglia the Regional Centre based at the Rosie Maternity Hospital operates informally. These centres are the responsibility of the regions concerned. They have built up considerable expertise over the years and regions will continue to have an interest in ensuring that their resident populations are best served by all the services that are purchased. Block contracting by purchasers simply means that access is given to a range of care at a specific price e.g. maternity and paediatrics, within which neonatal intensive care may or may not be separately identified. As the contracting process becomes more sophisticated, purchasers will begin to identify particular aspects of care separately and some are already doing this. Block contracts can be held at regional level and therefore their existence does not indicate any particular type of funding. In the first year of contracting for neonatal intensive care, the contracting arrangements have been largely based on the previous pattern of referrals and purchasers have been funded accordingly. Because of the expertise that has built up over the years in regional and sub-regional centres, these are even better placed than before in a system where the money follows the patient. As Dr Walford stated in her response to Q871, it is the purchasers’ responsibility to enter into the most appropriate contracts for their residents. In some cases, where residents live some distance from their own regional centres, this may even be with centres situated outside the region itself. (i) Babies admitted to neonatal intensive care units seem not to be being classified as ‘‘emergencies” and admissions are being charged as part of a block contract (Q860). Is it the Department’s policy that ill newborn babies are ““emergencies’’, and that potential disputes about payment should be avoided; and is it the expectation of the Department that the charge should be sensitive to the care given in future contracts?](https://iiif.wellcomecollection.org/image/b32222907_0031.jp2/full/800%2C/0/default.jpg)